Chronic fatigue syndrome — also known as myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) OR systemic exertional intolerance disease (SEID)— is a serious, chronic illness that can cause pain and extreme fatigue.
The Centers for Disease Control and Prevention (CDC) estimates that
In the past, some people did not believe that ME/CFS was a real illness. However, experts have started to take it more seriously in recent years, and research is underway to find out why it happens and how to treat it.
Lifestyle strategies and medical treatment may help people manage some of the symptoms.
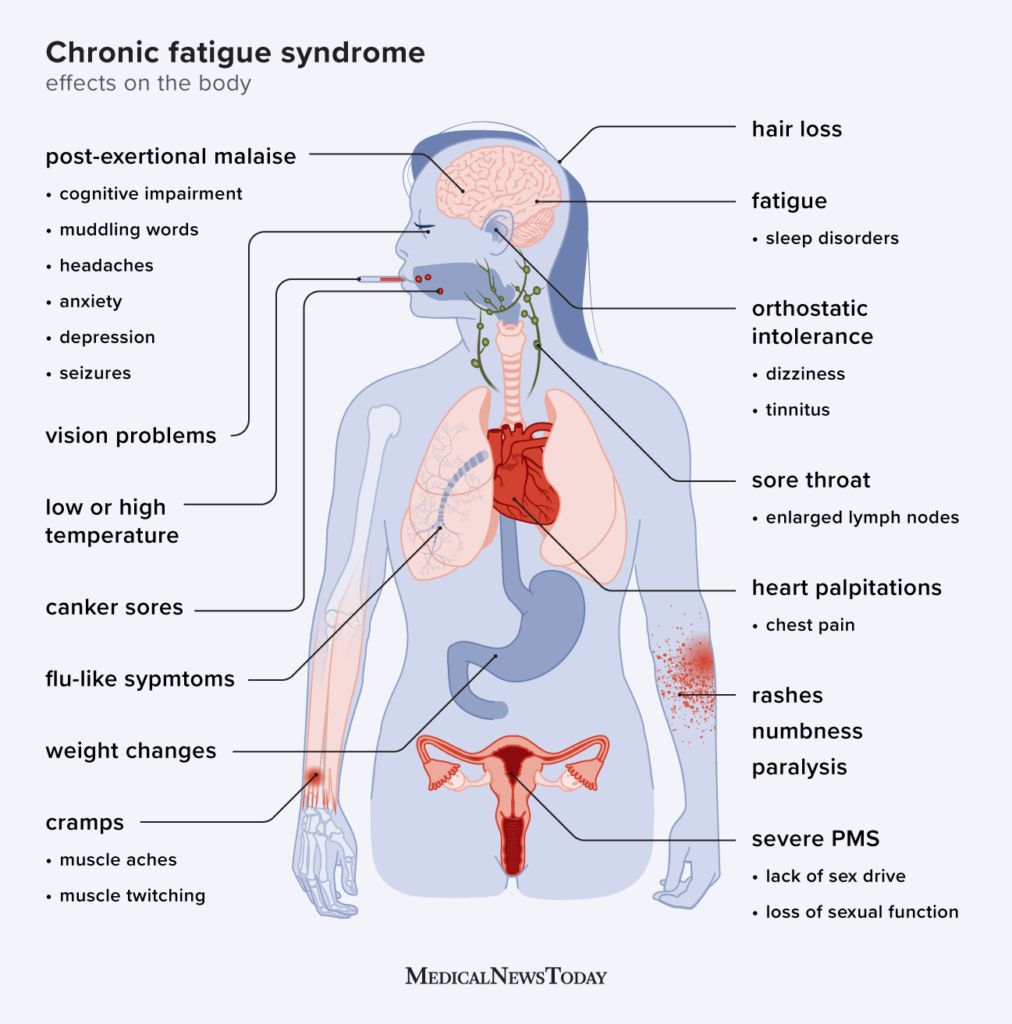
ME/CFS is a complex condition that can affect a range of bodily systems and functions.
Many of the possible symptoms resemble those of other conditions, making ME/CFS hard to diagnose.
The symptoms of ME/CFS can vary widely, but there are three core symptoms:
Reduced ability to function
A person with ME/CFS experiences fatigue that interferes with their ability to carry out daily tasks.
The fatigue:
- is severe
- does not improve with rest
- is not due to activity
- was not previously present
For a diagnosis of ME/CFS, this fatigue and the resulting decrease in activity levels must last
Post-exertional malaise
A person with post-exertional malaise (PEM) will experience a “crash” after physical or mental exertion.
During times of PEM, they may have new or worsening symptoms that include:
- difficulty thinking
- difficulty sleeping
- a sore throat
- headaches
- dizziness
- tiredness
Following an event that triggers PEM, the person may be unable to leave the house, get out of bed, or do regular chores for several days or even weeks. The symptoms tend to become worse
The trigger will depend on the individual. For some people, even having a shower or going to the grocery store can trigger PEM.
Sleep disorders
A range of sleep disorders can occur with ME/CFS. The person may feel very sleepy but be unable to sleep or not feel refreshed after sleeping. They may experience:
- intense and vivid dreaming
- restless legs
- nighttime muscle spasms
- sleep apnea
Other key symptoms
As well as the three core symptoms above, one of the following two symptoms must be present for a diagnosis of ME/CFS, according to the
- Problems with thinking and memory: People may experience “brain fog“, which includes problems with:
- making decisions
- focusing on details
- thinking quickly
- remembering things
- Dizziness when standing up: When the person moves from lying on their back to sitting or standing, they may experience:
- dizziness
- lightheadedness
- faintness
- vision changes, such as blurred vision or seeing spots
Other possible symptoms
Pain is a common symptom. A person with ME/CFS will often experience pain or discomfort that does not stem from an injury or other identifiable cause.
Common types of pain include:
- muscle aches and pains
- joint pain without redness or swelling
- headaches
The person may also experience:
- tenderness in the lymph nodes, especially the neck or armpits
- gastrointestinal problems
- chills and night sweats
- allergies to food
- sensitivity to light, touch, heat, or cold
- muscle weakness
- shortness of breath
- irregular heartbeat
- irritability and mood changes
- anxiety or panic attacks
- numbness, tingling, and burning in the hands, feet, and face
- eye pain
- a low grade fever
- vision problems
In addition, the American Myalgic Encephalomyelitis and Chronic Fatigue Syndrome Society (AMMES) notes that other possible symptoms include:
- muscle twitching
- rashes
- canker sores
- depression
- high stress levels
- saying words incorrectly
- tinnitus
- extreme symptoms of premenstrual syndrome (PMS)
- lack of sex drive or sexual impotence
- hair loss
- unexplained weight changes
- chest pain
- seizures
- paralysis
- spatial disorientation
- difficulty walking
- difficulty moving the tongue to form words
Experts do not know
- a flu-like illness
- a stomach bug or other infection
- the Epstein-Barr virus, which causes mononucleosis, commonly known as “mono”
- extreme physical stress, for example, surgery
There is growing
According to the Office on Women’s Health, females are
The symptoms of ME/CFS vary widely and can resemble those of other conditions, which can make it difficult to diagnose.
If a person seeks medical help for ME/CFS, a doctor will likely begin the diagnostic process by:
- asking about the person’s symptoms
- carrying out a physical examination
- recommending tests to try to identify the cause of any symptoms
To receive a diagnosis of ME/CFS, a person must have the three core symptoms of the condition for
It can take time to eliminate other possible causes of ME/CFS symptoms, but there is no specific test that can identify the condition.
In 2018,
In 2019, another research team announced that they had made further progress in developing a test. The test focused on certain features of blood cells and electrical activity in people with ME/CFS.
In the past, many doctors did not believe that ME/CFS was a real disease, but major health organizations now recognize it.
Various advocacy groups, including Solve M.E., are working to promote awareness of ME/CFS and empower people with the condition to persist in getting a diagnosis.
The AMMES list other advocacy groups on their website, provide useful resources, and explain where people can get support.
There is currently no cure or treatment specific to ME/CFS, but a doctor may work with individuals to help them manage the symptoms. The treatment plan
However, it
- focusing on whichever symptom poses the greatest challenge
- alleviating pain
- learning new ways to manage activities
Managing PEM
One way to manage fatigue after activity is through pacing or activity management.
The person will work with a doctor to determine the best way to balance rest and activity. The doctor will also help them identify their personal triggers and establish how much exertion they can tolerate.
Sleep
ME/CFS causes fatigue and can also disrupt sleep. A doctor will encourage the person to establish healthy sleeping habits, such as a regular sleep schedule.
If these strategies do not help, the doctor may prescribe medication.
Pain
At first, a doctor may recommend over-the-counter (OTC) drugs for headaches and other types of pain. If these do not work, they may prescribe stronger medication.
A person with ME/CFS may be sensitive to various chemicals. Therefore, they should speak with a doctor before using any new medication.
Nondrug therapies that may help include:
- gentle stretching and toning exercises
- gentle massage
- heat therapy
- water therapy
Anxiety and depression
Anxiety and depression are common among people with ME/CFS. Antidepressant drugs may help some people, but they can sometimes make symptoms worse.
Lifestyle remedies that may help include:
- relaxation techniques
- massage
- deep breathing
- gentle exercise, such as tai chi or yoga
Experimental medicines
Some laboratory
However, more research is necessary to ensure that the drug is safe to use in the treatment of this condition.
Various strategies can help people manage ME/CFS.
These include:
- finding a doctor who understands the condition
- seeking a counselor who can help manage the emotional and practical challenges
- making family and friends aware of the symptoms and challenges
- scheduling rest and activity times to maximize quality of life
- using calendars and journals to help with memory lapses
- learning which relaxation techniques are effective for them
- following a balanced and nutritious diet
- taking nutritional supplements if tests reveal a deficiency
- finding someone to help with child care and household chores at difficult times, if possible
What about exercise?
Gentle stretching, yoga, and tai chi might be helpful in some cases, and at the right time, but vigorous exercise can make symptoms worse.
The
People with symptoms or a diagnosis of ME/CFS should not follow any type of activity plan without discussing it with their doctor first.
Can I live a normal life with CFS?
ME/CFS affects people differently and can impact lives in different ways. People with mild ME/CFS may be able to go to work or school and function well in other areas of life, although they may need to plan their activities carefully and schedule plenty of rest.
People with moderate ME/CFS may have difficulty performing daily tasks and attending work or school. Those with severe impairment may need to use a wheelchair or spend a lot of time in bed. They will likely need help with daily activities. People may have severe impairment for
What foods should I avoid with chronic fatigue?
There is no research to suggest that limiting certain foods helps with CFS. However, if people have symptoms of irritable bowel at the same time, they can try to:
- eat a variety of fresh fruits and vegetables
- avoid sugary foods and refined grains, such as white bread and pasta
- choose slow-release carbohydrates, such as brown rice, oats, and starchy vegetables
- drink plenty of water or unsweetened beverages
- avoid alcohol
- cut out junk food
ME/CFS is a life changing condition that can affect every aspect of a person’s daily life.
It can take time to get a diagnosis, as the symptoms are not specific but overlap with those of other conditions. Whether or not a person has a diagnosis, lifestyle strategies can help them manage the challenges.
Until scientists find a specific treatment, coping strategies will play a key role in managing ME/CFS.