TRICARE for Life (TFL) is not a Medicare Advantage plan. It is secondary insurance to Medicare for active duty and ex-military members. The plan helps pay out-of-pocket healthcare costs, such as copays and coinsurance.
The TFL plan is not a Medicare Advantage plan, which is a primary health plan rather than secondary insurance. TRICARE, the company that offers TFL, does not offer any Advantage plans.
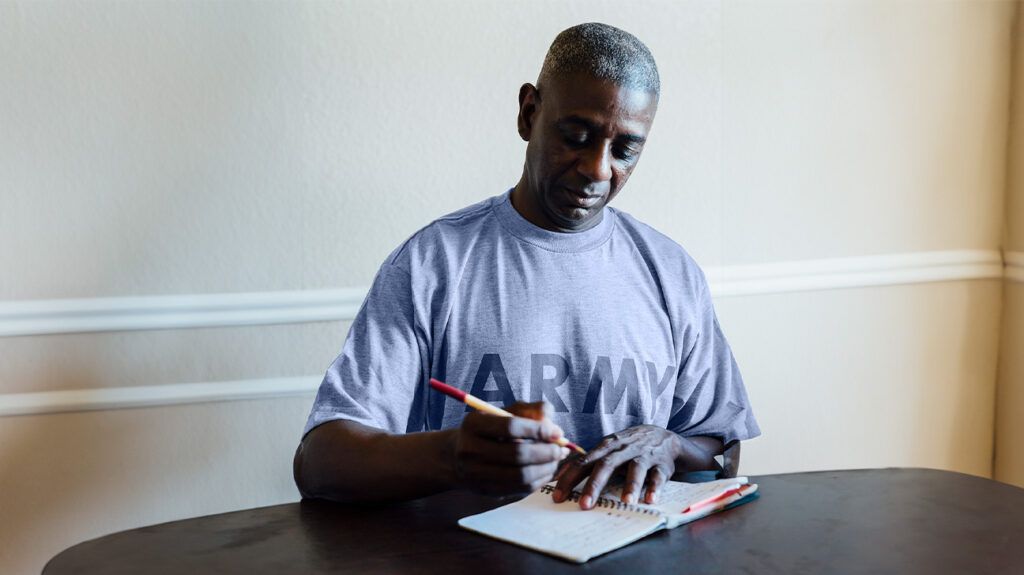
This article discusses the TRICARE for Life plan and also outlines TFL costs, eligibility, and enrollment information.
Glossary of Medicare terms
- Out-of-pocket cost: This is the amount a person must pay for care when Medicare does not pay the total amount or offer coverage. Costs can include deductibles, coinsurance, copayments, and premiums.
- Premium: This is the amount of money someone pays each month for Medicare coverage.
- Deductible: This is an annual amount a person must spend out of pocket within a certain period before Medicare starts to fund their treatments.
- Coinsurance: This is the percentage of treatment costs that a person must self-fund. For Medicare Part B, coinsurance is 20%.
- Copayment: This is a fixed dollar amount a person with insurance pays when receiving certain treatments. For Medicare, this usually applies to prescription drugs.
TFL is a federal government health insurance program for active duty and retired military personnel and their dependents.
TRICARE offers many health plans, including TRICARE Prime, TRICARE Extra, and TRICARE Standard. A person may use this online tool to find a plan that suits their needs.
However, the TFL plan is an option for those who are:
- Medicare-eligible uniformed services retirees ages 65 or older
- their eligible family members and survivors
- certain former spouses
- a person registered with the Defense Enrollment Eligibility Reporting System (DEERS)
- a Medal of Honor recipient or eligible family member
A person must also have enrollment in Original Medicare (parts A and B) to get TFL.
The TFL plan works as a supplement to Medicare. When a person with the plan visits a doctor, the doctor’s office files the claim with Medicare. After Medicare processes the claim and pays its portion, the bill goes to TFL, which often pays the remaining costs.
In other words, Medicare is the primary-payer insurance, and TFL is the second-payer insurance.
Medicare Advantage (Part C) is an alternative to Original Medicare (parts A and B). Private companies offer Advantage plans, which may include prescription drug coverage and other benefits such as dental and vision care.
Advantage plans have different out-of-pocket costs from Original Medicare. They also cap yearly expenses.
A person enrolled in TFL can also get an Advantage plan. However, there are factors to consider, including the following:
- Both TFL and many Advantage plans offer prescription drug coverage. Therefore, a person could choose an Advantage plan that does not offer prescription drug coverage as the premium may be lower, though there may still be copays.
- A person may need to pay a copay if they visit an in-network doctor through an Advantage plan. However, TFL may cover the cost.
- The in-network provider list for an Advantage plan may be smaller than a similar list for TFL or Original Medicare.
Find out who offers Medicare Advantage plans.
TFL does not charge any monthly premiums, although a person has to pay the Medicare Part B monthly premium, which is $174.70 in 2024. This amount may be more for people with a higher income.
Medicare pays 80% of the out-of-pocket costs, and TFL pays the remaining 20% and the Part B annual deductible of $240 in 2024. However, if a person goes to a healthcare professional who does not accept Medicare, they will be responsible for paying 80% of the cost, and TFL will pay the remaining 20%.
Because TFL covers prescription drugs, a person may have a copay charge but will not need to enroll in Medicare Part D, which is coverage for prescription drugs.
TLF does not cover some services, such as chiropractic care. For those services, Medicare pays 80%, and the insured person pays 20%. However, TFL covers most of the services that Medicare covers, and the combination of Medicare and TFL may provide for most of a person’s healthcare needs.
If someone has other health insurance (OHI), such as an employer-based health plan or Medicare supplement plan (Medigap), they can use TFL as long as they also have Original Medicare. Having OHI may alter the order in which insurers pay out.
If a person has employer-based insurance from a current employer:
- OHI pays its share first
- Medicare pays second
- TRICARE pays last
If a person has OHI that is not based on a person or their spouse’s current employment:
- Medicare pays first
- OHI pays second
- TRICARE pays last
Read more about when Medicare becomes a secondary payer.
There are two eligibility requirements for TFL: one related to Medicare and the other to the military. A person can check their eligibility online.
A person is eligible for TFL as soon as they enroll in Original Medicare.
An individual with Medicare is eligible for TFL if they fall into any of these categories:
- a retired serviceperson
- a spouse or dependent of a retired serviceperson
- a survivor of a deceased spouse who was a serviceperson
- a Medal of Honor recipient or eligible family member
- a person registered in DEERS
- an eligible former spouse of a serviceperson
Learn more about Medicare for veterans.
People do not need to fill out a form to enroll in TFL. They are automatically covered if they are enrolled in Original Medicare and registered in DEERS.
However, a person must have a valid military ID card, which they must renew after it expires on the first day of the month they turn 65.
The Social Security Administration (SSA) automatically enrolls eligible people who receive benefits in TFL. They can check their status by contacting their local SSA office or calling 800-772-1213.
If a person delays enrollment in Original Medicare, disenrolls from Medicare Part B, or stops paying Medicare Part B premiums, TFL suspends their coverage until they reenroll. Upon re-enrollment, a person will automatically receive TFL benefits again.
The TFL plan is available to eligible people across the United States and its territories, including Puerto Rico and Guam. A person who lives overseas in non-U.S. territories with an established military hospital may enroll in the TRICARE Overseas Program (TOP) TRICARE for Life.
Because Medicare is unavailable overseas, the TOP program functions as the primary insurer. People with the TOP plan must pay TRICARE’s yearly deductible and cost sharing. They are also responsible for any fees that exceed the plan’s allowable charges.
Medicare resources
For more resources to help guide you through the complex world of medical insurance, visit our Medicare hub.
TRICARE for Life (TFL) is a health insurance supplement that pays most of the out-of-pocket costs associated with Original Medicare. However, the company does not offer Advantage plans.
A person must be an Original Medicare enrollee and have military credentials, such as proof that they are a retired serviceperson, a surviving spouse, or one of their dependents, to get TFL benefits.
People with a TFL plan do not pay a monthly premium but must pay the Medicare Part B monthly premium.


