Xolair is a brand-name subcutaneous injection that’s prescribed for certain conditions, including asthma and hives. Xolair is a biologic that contains the active ingredient omalizumab.
Xolair is FDA approved to:
- treat moderate to severe allergic asthma in certain people ages 6 years and older
- treat chronic (long-lasting) hives with an unknown cause in certain people ages 12 years and older
- decrease allergic reactions from certain food allergies in people ages 1 year and older
- treat chronic sinus infection with nasal polyps in certain adults, along with other treatments
Note that Xolair should not be used for treating sudden asthma symptoms, such as shortness of breath, or hives with an unknown cause. It also should not be used for emergency treatment of allergic reactions, including anaphylaxis.
Drug details
Here you’ll find key information about Xolair.
- Drug class: monoclonal antibody
- Drug form: subcutaneous injection
- Generic or biosimilar available? no
- Prescription required? yes
- Controlled substance? no
- Year of FDA approval: 2003
Xolair contains the active ingredient omalizumab, which is a biologic medication. It’s available only as a brand-name medication. Xolair isn’t currently available in biosimilar form.
Biologic medications are made from living cells. A
It’s not possible to make an exact copy of a biologic. A generic, on the other hand, refers to a drug made from chemicals. A generic contains the same active ingredient that’s in the brand-name version.
Biosimilars are considered just as safe and effective as their parent drugs. And like generics, biosimilars tend to cost less than brand-name medications.
Xolair can cause mild or serious side effects. The following lists contain some of the key side effects that may occur while receiving Xolair. These lists do not include all possible side effects.
For more information on the possible side effects of Xolair, talk with your doctor or pharmacist. They can give you tips on how to manage any side effects that may be concerning or bothersome.
Note: After the Food and Drug Administration (FDA) approves a drug, it tracks and reviews side effects of the medication. Sharing your experience helps make medications safer for everyone by giving doctors and researchers more information about how the drug works in real life. If you develop a side effect while receiving Xolair and want to tell the FDA about it, visit MedWatch or call 800-332-1088.
Side effects of Xolair can vary depending on the condition you’re using the drug to treat. The more common side effects seen in Xolair’s clinical trials are described next.
More common side effects
The more common side effects of Xolair in people ages 12 years and older with allergic asthma can include:
- pain, which can be throughout the body, including in the joints, legs, and arms
- reactions near the injection site, which may cause pain or skin discoloration
- dizziness
- tiredness
- itchy skin
- skin rash
- bone fractures
- earache
The more common side effects of Xolair in people ages 12 years and older with chronic (long-lasting) hives can include:
- nausea
- nasopharyngitis (the common cold)
- sinus infection
- upper respiratory infection
- reactions near the injection site
- joint pain
- headache
- cough
- hair loss
To learn more about hair loss, see the “Side effect details” section.
The more common side effects of Xolair in children ages 1 to 17 years with food allergies can include:
- reactions near the injection site
- fever
These side effects were reported in a clinical trial of Xolair for food allergies that mainly included children. However, side effects are expected to be similar in adults taking the drug for this condition.
The more common side effects of Xolair in adults who have sinus infection with nasal polyps can include:
- headache
- reactions near the injection site
- pain in the joints or upper abdomen
- dizziness
Most of these side effects may go away within a few days to a couple of weeks. If they’re more severe or don’t go away, talk with your doctor or pharmacist.
Serious side effects
Serious side effects from Xolair aren’t common, but they can occur. Call your doctor right away if you have serious side effects. Call 911 or your local emergency number if your symptoms feel life threatening or if you think you’re having a medical emergency.
Serious side effects and their symptoms can include the following:
- Parasitic worm infection. Symptoms can include:
- abdominal pain
- diarrhea
- Heart and blood circulation problems, such as heart attack, stroke, and blood clots. Symptoms can include:
- pain in your chest
- being unable to speak clearly, for example, due to slurring
- feeling weak on one side of your body
- having changes in your vision
- Bone fractures.
- Immune system reaction, which may cause fever, rash, and joint pain.
Other serious side effects, which are discussed in more detail later, include:
- Cancer, which can include several types, such as:
- Anaphylaxis (a severe allergic reaction).
Xolair has a boxed warning from the Food and Drug Administration (FDA) regarding the risk of anaphylaxis. A boxed warning is the strongest warning the FDA requires. It alerts doctors and patients about drug effects that may be dangerous.
Side effects in children
The safety of Xolair in children was reported from clinical trials of children ages 6 to less than 12 years with allergic asthma and children ages 1 to 17 years with food allergies. The following side effects were reported in these clinical trials:
- nasopharyngitis (the common cold)
- headache
- fever
- pain in the upper abdomen
- strep throat
- ear infection
- viral gastroenteritis (the stomach flu)
- bloody nose
- bug bites
- reactions near the injection site
If you’re concerned about side effects in a child using Xolair, talk with the child’s doctor. They can recommend ways to help reduce these side effects during treatment.
Side effect details
You may wonder how often certain side effects occur with this drug, or whether certain side effects pertain to it. Here are some details on several of the side effects this drug may or may not cause.
Cancer
Some people have developed cancer while using Xolair. In clinical trials of people ages 12 years and older, some people using Xolair developed breast, skin, or prostate cancer.
In the clinical trials, cancer developed more often in people receiving Xolair than in people taking a placebo (a treatment with no active drug ingredient). However, in a trial of people with allergic asthma, those who were receiving Xolair had similar rates of cancer development as those who either took other asthma drugs or didn’t take any treatment at all. So it’s not clear whether Xolair may have increased the risk of cancer in clinical trials, or whether cancer developed due to other factors.
Symptoms of cancer can vary depending on what type of cancer you have. If you have concerns about your risk of developing cancer while using Xolair, talk with your doctor.
Allergic reaction, including anaphylaxis
As with most drugs, some people can have an allergic reaction after receiving Xolair. Symptoms of a mild allergic reaction can include:
A more severe allergic reaction, called anaphylaxis, is rare but possible. In fact, Xolair has a boxed warning from the Food and Drug Administration (FDA) about the risk of anaphylaxis. A boxed warning is the strongest warning the FDA requires. It alerts doctors and patients about possible side effects that may be dangerous.
Symptoms of anaphylaxis can include:
- swelling under your skin, typically in your eyelids, lips, hands, or feet
- swelling of your tongue, mouth, or throat
- difficulty breathing
- cough
- tightness in your chest
- flushing
- hives and itchiness
It’s possible to have anaphylaxis right after your Xolair injection, or days after your injection. This reaction can occur after just one dose of the drug or after many doses.
After you’re given Xolair by a healthcare professional, you’ll be monitored closely for this reaction.
If your doctor has you administer Xolair injections yourself, they’ll first consider your risk of anaphylaxis. And they’ll make sure you’re able to identify anaphylaxis and treat it right away.
In case of severe allergic reaction
Call your doctor right away if you have a severe allergic reaction to Xolair. Call 911 (or your local emergency number) if your symptoms feel life threatening or if you think you’re having a medical emergency.
If you’ve had a severe allergic reaction to Xolair, you shouldn’t continue using the drug. Your doctor will recommend a different medication for you to use instead of Xolair.
Hair loss
It’s possible to have hair loss while you’re receiving Xolair.
In clinical trials of people with chronic hives, hair loss occurred in a small percentage of people receiving Xolair. Hair loss was seen in a lower percentage of people taking a placebo (treatment with no active drug ingredient).
If you have concerns about hair loss while you’re using Xolair, talk with your doctor. They can recommend ways to help manage this condition.
As with all medications, the cost of Xolair can vary. The actual price you’ll pay depends on your insurance plan, your location, and the pharmacy you use.
Your healthcare professional may give you injections of Xolair in their office or clinic. Visits to your doctor’s office or clinic will likely come with additional costs. If your doctor recommends it, you may be able to give yourself Xolair injections at home.
If you and your doctor agree that you’ll give yourself Xolair injections, you’ll have to get Xolair at a specialty pharmacy. This type of pharmacy is authorized to carry specialty medications. These are drugs that may be expensive or may require help from healthcare professionals to be used safely and effectively.
Financial and insurance assistance: If you need financial support to pay for Xolair, or if you need help understanding your insurance coverage, help is available.
Copay programs and other resources are available for Xolair. For more information and to find out whether you’re eligible for support, call 866-4ACCESS (866-422-2377) or visit the drug website.
Generic or biosimilar version: Xolair is a biologic that’s not available in a
The Xolair dosage your doctor prescribes will depend on several factors. These include:
- the type and severity of the condition you’re using Xolair to treat
- your age
- your weight
- other medical conditions you may have
The following information describes dosages that are commonly used or recommended. However, be sure to take the dosage your doctor prescribes for you. Your doctor will determine the best dosage to fit your needs.
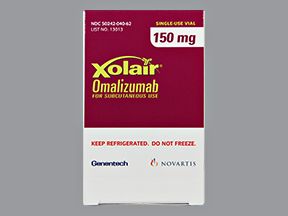
Drug forms and strengths
Xolair is available in the following strengths:
- 75 milligrams (mg) per 0.5 milliliters (mL), 150 mg/1 mL, and 300 mg/2 mL: These strengths each come as a liquid solution inside of:
- prefilled single-dose syringes
- prefilled auto-injector pens
- 150 mg: This strength comes as a powder that a healthcare professional mixes with liquid to form a solution. It comes in single-dose vials for use with a syringe. Only a healthcare professional can inject this form of Xolair.
All forms of Xolair are given by subcutaneous injection.
The maximum dose of Xolair that can be injected into one area of your body is 150 mg. If your dose of Xolair is greater than 150 mg, you’ll get more than one injection in different areas of your body. (For more information about injection sites, see the “How Xolair is given” section.)
Dosage for asthma
The typical dosage of Xolair for persistent (long-lasting) allergic asthma is 75 mg to 375 mg once every 2 or 4 weeks.
Your exact dosage will be based on your body weight and the results of a certain blood test that checks for an allergy marker called immunoglobulin E (IgE). Your doctor will order this test for you before you start receiving Xolair.
This is the recommended dosage for this condition in adults and children ages 12 years and older. For treating children ages 6 years to less than 12 years for this type of asthma, see the “Pediatric dosage” section.
Dosage for hives
The typical dosage of Xolair for chronic (long-lasting) hives with an unknown cause is either:
- 150 mg once every 4 weeks, or
- 300 mg once every 4 weeks
This is the recommended dosage for this condition in adults and children ages 12 years and older.
Dosage for food allergies
The typical dosage of Xolair for certain food allergies is 75 mg to 600 mg once every 2 or 4 weeks.
Your exact dosage will be based on your body weight and the results of an IgE blood test. Your doctor will order this test for you before you start Xolair treatment.
This is the recommended dosage for this condition in adults and children ages 1 year and older.
Dosage for sinus infection with nasal polyps
The typical dosage of Xolair for chronic rhinosinusitis (sinus infection) with nasal polyps is 75 mg to 600 mg once every 2 or 4 weeks.
Your exact dosage will be based on your body weight and the results of an IgE blood test. Your doctor will order this test for you before you start Xolair treatment.
This is the recommended dosage for this condition in adults.
Pediatric dosage
Pediatric dosages of Xolair vary, depending on the condition treated.
Children’s dosage for asthma
For persistent allergic asthma, children’s dosages vary, as shown in the following chart:
| For children ages 6 years to 11 years: | Xolair is typically given once every 2 to 4 weeks. The Xolair dosage will be based on body weight and the results of an IgE blood test. |
|---|---|
| For children ages 12 years and older: | Xolair is given in the same dosages as for adults. For this information, see the “Dosage for asthma” section. |
Children’s dosage for hives
For chronic hives, the typical dosage of Xolair is the same in children ages 12 years and older as it is in adults. For dosage information, see the “Dosage for hives” section.
Children’s dosage for food allergies
For certain food allergies, the typical dosage of Xolair is the same in children ages 1 year and older as it is in adults. For dosage information, see the “Dosage for food allergies” section.
What if I miss a dose?
If you miss an appointment for your dose of Xolair, call your healthcare professional’s office right away to schedule another injection.
If you give yourself Xolair injections at home, contact your doctor and ask how you should handle the missed injection.
To help you avoid missing a dose, try setting a reminder on your phone or leaving a note for yourself on your calendar.
Will I need to use this drug long term?
Xolair is meant to be used as a long-term treatment. If you and your doctor determine that Xolair is safe and effective for you, you’ll likely use it long term. You doctor will monitor your symptoms and recommend whether you should continue treatment with Xolair.
The Food and Drug Administration (FDA) has also approved Xolair to treat a certain type of asthma in adults and children ages 6 years and older.
Xolair is used to treat asthma that has all of these characteristics:
- It causes moderate to severe symptoms.
- It’s persistent (long-lasting).
- It’s considered allergic asthma, which is diagnosed by having a positive skin or blood test for allergens that are present year-round.
- It didn’t improve after treatment with other drugs called inhaled corticosteroids.
Symptoms of allergic asthma can occur when you breathe in allergens, such as pet dander or dust mites. Some allergens are around throughout the year. Sometimes allergens can trigger your asthma symptoms to flare up (also called an asthma attack).
Symptoms of asthma that may occur include:
- difficulty breathing
- tightening in your chest
- coughing
- wheezing
For more information about asthma, you can refer to our asthma and allergies hub.
It’s important to note that Xolair shouldn’t be used to treat sudden asthma symptoms, such as shortness of breath. Instead, you should use a rescue inhaler for these symptoms. To learn more, see the “Xolair use with other drugs” section.
Effectiveness
Xolair has been found effective in treating allergic asthma when it’s used with other asthma medications called inhaled corticosteroids (ICS). After 16 weeks of treatment in clinical trials, more people using Xolair experienced no asthma attacks, compared with people using a placebo (treatment with no active drug ingredient).
In clinical trials, people were also taking an ICS drug. Healthcare professionals lowered the dosage of the ICS drug to determine whether it would be safe to decrease the amount of steroid that people receiving Xolair were taking. As the dosage of ICS was lowered, most people continued to have no asthma attacks.
The Food and Drug Administration (FDA) has approved Xolair to treat a type of hives called chronic spontaneous urticaria in adults and children ages 12 years and older. It’s used in people whose hives aren’t managed with certain antihistamines called H1 antihistamines.
Chronic spontaneous urticaria used to be called chronic idiopathic urticaria (CIU). It’s a condition that has all of these characteristics:
- It’s chronic (lasts a long time): It may occur every day, and it lasts for 6 weeks or longer.
- It has no known cause (called spontaneous or idiopathic): With this condition, certain blood or skin tests haven’t shown the cause of your hives. (If the cause of your hives is found, you may be prescribed a medication other than Xolair for treatment.)
- It results in hives (urticaria): Hives are small bumps on your skin that usually feel itchy. They’re sometimes called wheals or welts.
When H1 antihistamines no longer work to treat your hives, Xolair may be an option for you. This drug helps to relieve itchiness and reduce your hives.
It’s important to note that Xolair should not be used to treat other forms of hives.
Effectiveness
In clinical trials, Xolair reduced itchiness and decreased the hives people had. These reductions were more significant in people using Xolair than in people using a placebo (treatment with no active drug ingredient).
The Food and Drug Administration (FDA) has also approved Xolair to help decrease reactions from certain food allergies in people ages 1 year and older.
Specifically, Xolair helps decrease allergic reactions from accidental exposure to certain foods in people with IgE-mediated food allergies. IgE stands for immunoglobulin E, which is a type of antibody. In some people, certain foods may trigger an allergic response caused by these antibodies.
Not all food allergies are caused by IgE antibodies. Xolair is not FDA approved for food allergies that aren’t caused by IgE antibodies. Also, the drug does not enable people to consume foods to which they are allergic. The manufacturer recommends avoiding foods that can trigger an allergic reaction while receiving Xolair.
Symptoms of food allergies may include:
- nausea or vomiting
- diarrhea
- hives
- swelling
- wheezing
It’s important to note that Xolair should not be used as an emergency treatment for allergic reactions, including anaphylaxis (a severe allergic reaction).
Effectiveness
A clinical trial has found Xolair safe and effective for helping decrease allergic reactions due to IgE-mediated food allergies in adults and children ages 1 year and older. For details about this trial, see the Xolair prescribing information.
The Food and Drug Administration (FDA) has also approved Xolair to treat chronic (long-lasting) rhinosinusitis (sinus infection) with nasal polyps in adults.
The drug is used in adults whose condition hasn’t improved with nasal corticosteroids. And it’s given in combination with other treatments for this condition.
Chronic sinus infection is a condition that causes inflammation in the sinuses or nasal passages. This inflammation lasts for 12 weeks or more. Symptoms may include:
- blockage of nasal passages, which can cause difficulty breathing
- nasal discharge
- pain in areas of the face or mouth
Nasal polyps are noncancerous growths that form inside the nose or sinuses. These growths may not cause symptoms in some people. But possible symptoms of nasal polyps include:
- stuffy or runny nose
- altered sense of smell or taste
- facial pain
- breathing problems
Effectiveness
In clinical trials, Xolair was effective at treating sinus infection with nasal polyps in certain people. To learn how the drug performed in these studies, check out Xolair’s prescribing information.
The Food and Drug Administration (FDA) approves prescription drugs such as Xolair to treat certain conditions. To learn about Xolair’s approved uses, see the following sections:
- “Xolair for allergic asthma”
- “Xolair for urticaria (hives)”
- “Xolair for food allergies“
- “Xolair for sinus infection with nasal polyps”
Xolair may also be used off-label for other conditions. Off-label use is when a drug that’s approved to treat one condition is used to treat a different condition.
Xolair for allergies (off-label use)
Xolair is not FDA approved to treat allergic rhinitis (a type of allergy that’s also called hay fever). However, sometimes it’s prescribed off-label to treat this condition. Allergic rhinitis causes symptoms such as:
- congestion (stuffy nose)
- runny nose
- sneezing
- itchy eyes, nose, and throat
- watery eyes
Effectiveness for allergies
Studies have looked at using Xolair to treat both perennial (year-round) and seasonal allergic rhinitis.
In one study, Xolair was given to people with moderate to severe perennial allergic rhinitis. After 16 weeks of treatment, Xolair was more effective than a placebo in reducing people’s daily allergy symptoms. (A placebo is a treatment with no active drug ingredient.)
Another study found that omalizumab helped manage symptoms in people with moderate to severe allergic rhinitis. (Omalizumab is the active ingredient in Xolair.)
If you’re interested in using Xolair to treat allergies, talk with your doctor. They can discuss all of your treatment options with you.
Xolair for eczema (off-label use)
Xolair isn’t approved to treat atopic dermatitis (a type of eczema). But sometimes it’s prescribed off-label for this condition. This condition causes your skin to feel dry and itchy.
A
If you’re interested in using Xolair to treat eczema, talk with your doctor. They can discuss all of your treatment options with you.
Here are answers to some frequently asked questions about Xolair.
Is Xolair an immunosuppressant? Will it weaken my immune system?
Xolair isn’t classified as an immunosuppressant, and it isn’t believed to weaken your immune system.
Infections were reported as a side effect by some people receiving Xolair in clinical trials. This may make it seem like the drug reduces the immune system’s ability to fight off infection. However, it’s important to keep in mind that people with asthma and sinus infection with nasal polyps have a higher risk of infection than is typical. (These are two of the conditions that Xolair is used to treat.)
Research suggests that Xolair does not reduce immune system activity. (Omalizumab is the active ingredient in Xolair.)
If you’re concerned about how Xolair may affect your immune system, talk with your doctor. They can discuss with you the risks and benefits of using this drug.
Will I have withdrawal symptoms if I stop receiving Xolair?
Stopping Xolair isn’t known to cause withdrawal symptoms. These are symptoms that can occur if you stop taking a drug that your body has become dependent on. (With dependence, your body needs the drug in order to function like usual.)
However, stopping Xolair can cause symptoms of your condition to return. Because of this, you should talk with your doctor before stopping Xolair or any other medications. Your doctor can recommend whether it’s safe to do so.
Can I use Xolair for angioedema?
No, you shouldn’t use Xolair to treat angioedema (swelling caused by a severe allergic reaction). This drug isn’t approved to treat angioedema.
In fact, angioedema has been reported as a serious side effect of Xolair. And there haven’t been any studies done to look at using Xolair to treat the condition.
If you have questions about how to treat angioedema, talk with your doctor.
Is Xolair a type of chemotherapy?
No, Xolair isn’t chemotherapy (traditional drugs used to treat cancer). Its mechanism of action (how it works) is different from that of chemotherapy. (For more information, see the “How Xolair Works” section.)
Chemotherapy drugs use powerful chemicals to kill cells that are multiplying (making more cells) quickly in the body. Chemotherapy is effective for cancer treatment because cancer cells multiply more quickly than most other cells in the body.
Xolair is a monoclonal antibody. This type of drug is made in a lab using immune system cells. Monoclonal antibodies are used to treat various conditions. Some are used to treat certain forms of cancer. However, Xolair is not approved to treat cancer.
If you have questions about cancer treatment options, talk with your doctor.
Does Xolair contain steroids?
No, Xolair isn’t a steroid and it’s not made from steroids. Xolair is a monoclonal antibody. These drugs are made in a lab from immune system cells. They work differently in your body than steroids do.
Your doctor may recommend that you use a corticosteroid along with Xolair. (This could be a corticosteroid that’s either inhaled, taken by mouth, or sprayed into your nose.) This combination of drugs is sometimes prescribed to better treat your condition.
Can Xolair cause depression?
Studies haven’t shown that Xolair causes or leads to depression. However, you may have a higher risk of depression if you have persistent asthma or chronic hives. Xolair is prescribed to treat both of these conditions.
Living with these long-term conditions may lead to changes in your emotions. If you feel depressed during treatment with Xolair, talk with your doctor. They’ll recommend ways to help manage your mood, and they can help you decide whether to get treatment for your symptoms.
Other drugs are available that can treat your condition. Some may be better suited for you than others. If you’re interested in finding an alternative to Xolair, talk with your doctor. They can tell you about other medications that may work well for you.
Note: Some of the drugs listed here are prescribed off-label to treat these specific conditions. Off-label use is when a drug that’s approved to treat one condition is prescribed to treat a different condition.
Alternatives for asthma
Examples of other drugs that may be used to treat moderate to severe allergic asthma that’s persistent (long-lasting) include:
- certain oral corticosteroids, such as:
- prednisone
- methylprednisolone (Medrol)
- leukotriene modifiers, such as:
- montelukast (Singulair)
- zafirlukast (Accolate)
- zileuton (Zyflo)
- other biologic medications, such as:
Alternatives for hives
Examples of other drugs that may be used to treat chronic idiopathic urticaria (hives with an unknown cause) include:
- certain oral corticosteroids that are used for a short time to reduce symptoms, such as:
- prednisone
- methylprednisolone (Medrol)
- doxepin (Zonalon), a tricyclic antidepressant drug that comes as a topical cream
- certain immunosuppressants (drugs that suppress your immune system), such as:
- cyclosporine (Neoral, Gengraf)
- tacrolimus (Prograf)
Alternatives for food allergies
Currently, Xolair is the only FDA-approved drug used to help reduce allergic reactions caused by different foods before they happen. However, there is one drug, peanut allergen powder-dnfp (Palforzia), that is FDA approved to help reduce allergic reactions caused by peanuts.
The following medications are available for treating symptoms of allergic reactions due to food allergies:
- antihistamines, such as diphenhydramine (Benadryl) or loratadine (Claritin), for mild to moderate reactions
- epinephrine (EpiPen), for severe reactions
Alternatives for sinus infection with nasal polyps
Examples of other drugs that may be used to treat sinus infection with nasal polyps include:
- corticosteroid nasal sprays, such as:
- fluticasone (Flonase Allergy Relief)
- triamcinolone (Nasacort Allergy 24 Hour)
- leukotriene modifiers, such as:
- montelukast (Singulair)
- zafirlukast (Accolate)
- zileuton (Zyflo)
You should use Xolair according to your doctor’s or another healthcare professional’s instructions.
When to use
Xolair is given as a subcutaneous injection. Your doctor or another healthcare professional will administer your Xolair doses when you first start treatment.
In some cases, your doctor may recommend that you self-inject doses of the drug at home. But you’ll receive at least your first three Xolair doses at a healthcare facility.
In either case, your doctor will recommend how often you need to have Xolair injections, depending on the condition you’re treating.
Xolair injection sites
Xolair can be injected into the following areas:
- thighs
- abdomen, avoiding the 2-inch area around the belly button
If a healthcare professional or caregiver injects Xolair, they can also inject it into the outer side of the upper arms.
You may wonder how Xolair compares with other medications that are prescribed for similar uses. Here we look at how Xolair and Dupixent are alike and different.
About
Xolair contains the drug omalizumab, while Dupixent contains the drug dupilumab. Both drugs are monoclonal antibodies, which means they’re made in a lab from immune system cells. However, Xolair and Dupixent each work differently inside your body.
Uses
The Food and Drug Administration (FDA) has approved Xolair and Dupixent to treat asthma.
Xolair is used to treat moderate to severe asthma that’s persistent (long-lasting). For this condition, Xolair is used in people ages 6 years and older who have both:
- allergic asthma, which is diagnosed by having a positive skin or blood test for allergens that are present year-round, and
- asthma symptoms that aren’t managed by other medications called inhaled corticosteroids
Dupixent is also used to treat moderate to severe asthma. It’s prescribed as a maintenance (long-term) treatment in combination with another asthma treatment. Dupixent is used in adults and children ages 6 years and older who:
- need to use drugs called oral corticosteroids for their asthma, or
- have a certain type of asthma called eosinophilic asthma
The FDA has also approved Xolair and Dupixent to treat sinus infection with nasal polyps in combination with other treatments for this condition.
For this purpose, Xolair is used in adults whose condition hasn’t improved with nasal corticosteroids. Dupixent is approved to treat sinus infection with nasal polyps in adults and children ages 12 years and older whose condition hasn’t been managed with other treatments.
Xolair and Dupixent also have approved uses that differ. For more information about other Xolair uses, see the “Xolair for urticaria (hives)” and “Xolair for food allergies” sections. To learn more about Dupixent’s other uses, talk with your doctor.
Drug forms and administration
Both Xolair and Dupixent are given by subcutaneous injection. Xolair and Dupixent injections may be given by a healthcare professional or self-injected at home. Your doctor will recommend how you should receive either drug.
Xolair is given once every 2 to 4 weeks. Dupixent is given once every week, every 2 weeks, or every 4 weeks.
Side effects and risks
Xolair and Dupixent both contain monoclonal antibodies. Therefore, these medications can cause very similar side effects.
More common side effects
The following table contains examples of more common side effects that can occur with Xolair, with Dupixent, or with both drugs (when received individually) when used to treat asthma or sinus infection with polyps.
| Mild side effect | Xolair | Dupixent |
|---|---|---|
| dizziness | ✓ | |
| tiredness | ✓ | |
| itchy skin | ✓ | |
| skin rash | ✓ | |
| bone fractures | ✓ | |
| earache | ✓ | |
| pain throughout the body | ✓ | |
| upper abdominal pain | ✓ | |
| increased level of eosinophils (a type of white blood cell) in the blood | ✓ | |
| pain in the mouth and throat | ✓ | |
| insomnia | ✓ | |
| toothache | ✓ | |
| reactions near the injection site, which may cause pain or skin discoloration | ✓ | ✓ |
| joint pain | ✓ | ✓ |
| headaches | ✓ | ✓ |
Serious side effects
The following table contains examples of serious side effects that can occur with Xolair, with Dupixent, or with both drugs (when received individually).
| Serious side effect | Xolair | Dupixent |
|---|---|---|
| cancer | ✓ | |
| problems with heart and blood circulation, such as heart attack, stroke, and blood clots | ✓ | |
| immune system reactions, which may cause fever, rash, and joint pain | ✓ | |
| inflammation in certain parts of the eye, such as the conjunctiva or cornea | ✓ | |
| inflammation of the blood vessels | ✓ | ✓ |
| parasitic worm infections | ✓ | ✓ |
| severe allergic reaction, including anaphylaxis | ✓ | ✓ |
Note: Xolair has a boxed warning from the Food and Drug Administration (FDA) regarding the risk of anaphylaxis (a severe allergic reaction). A boxed warning is the strongest warning the FDA requires. It alerts doctors and patients about drug effects that may be dangerous. For more information, see “Allergic reaction, including anaphylaxis” in the “Xolair side effects” section.
Effectiveness
Xolair and Dupixent have different FDA-approved uses, but they’re both used to treat asthma and sinus infection with polyps.
These drugs haven’t been directly compared in clinical trials. But separate studies have found both Xolair and Dupixent to be effective for treating moderate to severe asthma.
Costs
Xolair and Dupixent are both brand-name drugs. There are currently no generic or biosimilar forms of either drug. Brand-name medications usually cost more than generics. To learn more about generics and biosimilars, see the “Xolair generic or biosimilar” section.
The actual price you’ll pay for either drug depends on your insurance plan, your location, and the pharmacy you use.
While there aren’t any known interactions between Xolair and alcohol, you should talk with your doctor before drinking alcohol while you’re using this medication.
Alcohol can have various effects on your health. For example, alcohol can affect the way your immune system works. This can increase your risk of developing certain types of cancer or infections. Alcohol may also increase your risk of certain side effects of Xolair, such as dizziness, because both Xolair and alcohol can cause this.
If you drink alcohol, talk with your doctor about whether it is safe to consume while you’re using Xolair.
You may wonder how Xolair compares with other medications that are prescribed for similar uses. Here we look at how Xolair and Nucala are alike and different.
About
Xolair contains the drug omalizumab, while Nucala contains the drug mepolizumab. Both drugs are monoclonal antibodies, which means they’re made in a lab from immune system cells. However, Xolair and Nucala each work differently inside your body.
Uses
Xolair and Nucala are both approved to treat asthma.
Xolair is used to treat moderate to severe asthma that’s persistent (long-lasting). For this condition, Xolair is used in people ages 6 years and older who have both:
- allergic asthma, which is diagnosed by having a positive skin or blood test for allergens that are present year-round, and
- asthma symptoms that aren’t managed by other medications called inhaled corticosteroids
Nucala is used to treat severe forms of eosinophilic asthma. For this condition, it’s used in combination with other asthma treatments. It’s approved for this use in people ages 6 years and older.
The FDA has also approved Xolair and Dupixent to treat sinus infection with nasal polyps in combination with other treatments for this condition. For this purpose, each of these drugs is used in adults whose condition hasn’t improved with nasal corticosteroids.
Xolair and Nucala also have approved uses that differ. For more information about other Xolair uses, see the “Xolair for urticaria (hives)” and “Xolair for food allergies” sections. To learn more about Nucala’s other uses, talk with your doctor.
Drug forms and administration
Both Xolair and Nucala are given by subcutaneous injection. Xolair and Nucala injections may be given by a healthcare professional or self-injected at home. Your doctor will recommend how you should receive either drug.
Xolair is given once every 2 to 4 weeks, while Nucala is given once every 4 weeks.
Side effects and risks
Xolair and Nucala both contain monoclonal antibodies. Therefore, these medications can cause very similar side effects.
More common side effects
The following table contains examples of more common side effects that can occur with Xolair, with Nucala, or with both drugs (when received individually) when used to treat asthma or sinus infection with polyps.
| Mild side effect | Xolair | Nucala |
|---|---|---|
| dizziness | ✓ | |
| itchy skin | ✓ | |
| skin rash | ✓ | |
| bone fractures | ✓ | |
| earache | ✓ | |
| pain throughout the body | ✓ | |
| back pain | ✓ | |
| pain in the mouth and throat | ✓ | |
| reactions near the injection site, which may cause pain or skin discoloration | ✓ | ✓ |
| joint pain | ✓ | ✓ |
| headaches | ✓ | ✓ |
| upper abdominal pain | ✓ | ✓ |
Serious side effects
This table contains examples of serious side effects that can occur with Xolair, with Nucala, or with both drugs (when received individually).
| Serious side effect | Xolair | Nucala |
|---|---|---|
| cancer | ✓ | |
| problems with heart and blood circulation, such as heart attack, stroke, and blood clots | ✓ | |
| immune system reactions, which may cause fever, rash, and joint pain | ✓ | |
| inflammation of the blood vessels | ✓ | |
| shingles infection (caused by herpes zoster virus) | ✓ | |
| parasitic worm infections | ✓ | ✓ |
| severe allergic reaction, including anaphylaxis | ✓ | ✓ |
Note: Xolair has a boxed warning from the Food and Drug Administration (FDA) regarding the risk of anaphylaxis (a severe allergic reaction). A boxed warning is the strongest warning the FDA requires. It alerts doctors and patients about drug effects that may be dangerous. For more information, see “Allergic reaction, including anaphylaxis” in the “Xolair side effects” section.
Effectiveness
Xolair and Nucala have different FDA-approved uses, but they’re both used to treat asthma and sinus infection with nasal polyps.
These drugs haven’t been directly compared in clinical trials. But separate studies have found both Xolair and Nucala to be effective for treating severe asthma.
Costs
Xolair and Nucala are both brand-name drugs. There are currently no generic or biosimilar forms of either drug. Brand-name medications usually cost more than generics. To learn more about generics and biosimilars, see the “Xolair generic or biosimilar” section.
The actual price you’ll pay for either drug depends on your dosage, your insurance plan, your location, and the pharmacy you use.
It’s unknown whether Xolair is safe to receive during pregnancy or breastfeeding. If you have questions about receiving Xolair during pregnancy or while breastfeeding, talk with your doctor.
Xolair works with your immune system to:
- treat moderate to severe allergic asthma
- treat chronic (long-lasting) hives with an unknown cause
- decrease allergic reactions from IgE-mediated food allergies
- treat chronic sinus infection with nasal polyps, along with other treatments
With these conditions, your body has increased levels of a certain immune system protein called immunoglobulin E (IgE).
What is immunoglobulin E and what does it do?
IgE is an immune system protein that causes inflammation in your body.
If you have allergic asthma, IgE levels increase when you inhale allergens such as pet dander or dust mites. (Allergens are substances that cause allergies.) When IgE attaches to allergens, it causes other substances to be released inside your body. This leads to inflammation, which can narrow your airways and make it hard for you to breathe.
If you have chronic hives, IgE binds to mast cells (a type of white blood cell) in your skin. Once IgE attaches to mast cells, the cells cause other substances (such as histamine) to be released in your body. This leads to hives and itchy skin.
If you have IgE-mediated food allergies, proteins in certain foods act as allergens. When you eat such foods, IgE levels in your body increase, triggering an immune system response. Symptoms include nausea, diarrhea, hives, and swelling.
It’s not exactly known what causes sinus infection with nasal polyps. It’s thought that, similar to IgE, eosinophils cause inflammation in the body. (Eosinophils are a type of white blood cell.) This includes inflammation inside the nose. And this inflammation plays a role in nasal polyps forming.
What Xolair does
Xolair contains the drug omalizumab. It’s both a biologic drug and a monoclonal antibody. Biologics are drugs that are made from living cells, while monoclonal antibodies are drugs that are made from immune system cells.
Xolair’s mechanism of action (how it works) is by blocking IgE from binding to its receptors (attachment sites).
In people with asthma, Xolair decreases the amount of certain substances in their body that cause inflammation and asthma symptom flare-ups.
In people with chronic hives, Xolair lowers the amount of IgE that can attach to mast cells in their skin and cause inflammation.
In people with IgE-mediated food allergies, Xolair reduces the level of IgE, helping decrease symptoms of an allergic reaction caused by certain foods.
In people with sinus infection with nasal polyps, Xolair lowers IgE levels. This decreases inflammation, which is thought to help treat sinus infection with nasal polyps.
How long does it take to work?
It takes a little while for Xolair to begin to work in your body. You might not notice an improvement in your symptoms until you’ve used the drug for several months.
There haven’t been any studies done to look at whether Xolair interacts with any other drugs.
However, before starting Xolair, talk with your doctor and pharmacist. Tell them about all prescription, over-the-counter, and other drugs you take. Also, tell them about any vitamins, herbs, and supplements you use. Sharing this information can help you avoid potential interactions.
If you have questions about drug interactions that may affect you, ask your doctor or pharmacist.
Xolair and herbs and supplements
There aren’t any herbs or supplements that have been specifically reported to interact with Xolair. However, you should still check with your doctor or pharmacist before using any of these products while receiving Xolair.
Xolair and foods
There aren’t any foods that are known to interact with Xolair. However, if you have concerns about food interactions with this medication, talk with your doctor or pharmacist.
Xolair and lab tests
Xolair may increase your level of immunoglobulin E (IgE), which is an immune system protein. And this level can stay elevated for up to a year after you’ve stopped Xolair treatment.
If you use or have used Xolair, let your doctor know if they recommend you have a blood test to check your IgE level.
Xolair may be used with other drugs to treat your condition. Depending on the condition you’re using Xolair to treat, your doctor will recommend which medications you’ll need to use with Xolair.
Drugs used with Xolair for asthma
If you have moderate to severe allergic asthma that’s persistent (long lasting), your doctor may recommend taking other drugs with Xolair. Some drugs are used for quick relief of symptoms (called rescue medications), while other drugs are used for long-term symptom management.
Rescue medications for allergic asthma
Xolair is not a rescue medication. It’s not meant to be used to treat sudden breathing problems or asthma flare-ups. You’ll still need to use your rescue medication for quick relief of asthma symptoms while you’re receiving Xolair.
Examples of rescue medications that are used to quickly relieve asthma symptoms include:
- albuterol (ProAir HFA, Ventolin HFA)
- levalbuterol (Xopenex HFA)
Long-term medications for allergic asthma
Xolair may be used with other asthma medications for long-term management of asthma symptoms. Examples of these medications include:
- inhaled corticosteroids, such as:
- fluticasone (Flovent HFA)
- budesonide (Pulmicort Flexhaler)
- mometasone (Asmanex Twisthaler)
- beclomethasone (Qvar RediHaler)
- ciclesonide (Alvesco)
- long-acting beta-agonists (LABAs), such as:
- salmeterol (Serevent)
- combination medications (contain both a corticosteroid and LABA), such as:
- fluticasone/salmeterol (Advair Diskus)
- budesonide/formoterol (Symbicort)
- mometasone/formoterol (Dulera)
- fluticasone/vilanterol (Breo Ellipta)
- leukotriene modifiers, such as:
- montelukast (Singulair)
- zafirlukast (Accolate)
- zileuton (Zyflo)
Drugs used with Xolair for hives
If you have chronic (long-lasting) hives, you’ll most likely take an antihistamine with Xolair. Examples of nondrowsy and less-drowsy antihistamines include:
If your hives don’t improve after using one of these antihistamines with Xolair, your doctor may increase your dosage of the antihistamine. Or your doctor may recommend that you use a different type of antihistamine that may cause drowsiness, such as diphenhydramine (Benadryl).
Your doctor may also suggest that you use corticosteroid creams with Xolair. These could include creams such as betamethasone dipropionate (Diprolene), which you apply to your skin.
Drugs used with Xolair for food allergies
If you take Xolair to help decrease allergic reactions from IgE-mediated food allergies, you may take antihistamines to help ease symptoms of a mild allergic reaction. Examples of antihistamines include:
- loratadine (Claritin)
- desloratadine (Clarinex)
- fexofenadine (Allegra)
- cetirizine (Zyrtec)
For a severe allergic reaction from food allergies, your doctor will likely recommend that you carry epinephrine (EpiPen) with you in case of emergencies.
It’s important to note that Xolair should not be used as an emergency treatment for allergic reactions, including anaphylaxis (a severe allergic reaction).
Drugs used with Xolair for sinus infection with nasal polyps
If you have chronic sinus infection with nasal polyps, you’ll use Xolair in combination with another treatment. These may include:
- corticosteroid nasal sprays, such as:
- fluticasone (Flonase Allergy Relief)
- triamcinolone (Nasacort Allergy 24 Hour)
- leukotriene modifiers, such as:
- montelukast (Singulair)
- zafirlukast (Accolate)
- zileuton (Zyflo)
This drug comes with several warnings.
FDA warning: Anaphylaxis (severe allergic reaction)
This drug has a boxed warning. This is the most serious warning from the Food and Drug Administration (FDA). A boxed warning alerts doctors and patients about drug effects that may be dangerous.
Using Xolair can lead to a dangerous condition called anaphylaxis. This condition may occur after just one dose, or after many doses of Xolair. It may also occur right away after your dose or days later. After you’re given Xolair, you’ll be monitored closely for this reaction by your healthcare professional.
Your doctor may have you administer Xolair injections to yourself. They’ll consider your risk of anaphylaxis when determining whether this is safe. And they’ll make sure you’re able to identify anaphylaxis and treat it right away.
Anaphylaxis can include symptoms such as swelling of your tongue and throat, difficulty breathing, tightening in your chest, and low blood pressure. Anaphylaxis can also cause you to feel warm and itchy, or to have hives. If you have any of these symptoms, you need medical attention right away.
Other warnings
Before starting Xolair, talk with your doctor about your health history. Xolair may not be right for you if you have certain medical conditions or other factors. These include:
- cancer
- steroid treatment
- high risk of parasitic infection
- latex allergy
- previous severe allergic reaction to Xolair
- sudden breathing problems
- pregnancy or planned pregnancy
Disclaimer: Medical News Today has made every effort to make certain that all information is factually correct, comprehensive, and up to date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or another healthcare professional before taking any medication. The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.